Individuals who survive an infection normally become immune to that particular disease, although not to other diseases. This is because the immune system “remembers” foreign antigens, a process called immune memory . Next time the same antigen appears, it triggers a far swifter and more aggressive response than before. Consequently, the invading microorganisms will usually be overwhelmed before they cause noticeable illness. Immune memory is due to specialized B cells called memory cells . As discussed earlier, virgin B cells are triggered to divide if they encounter an antigen that matches their own individual antibody. Most of the new B cells are specialized for antibody synthesis, and they live only a few days. However, a few active B cells become memory cells, and instead of making antibodies, they simply wait. If one day the antigen they recognize appears again, most of the memory cells switch over very rapidly to antibody production. Vaccination takes advantage of immune memory. Vaccines consist of various derivatives of infectious agents that no longer cause disease but are still antigenic, that is, they induce an immune response. For example, bacteria killed by heating are sometimes used. The antigens on the dead bacteria stimulate B-cell division. Some of the B cells form memory cells so, later, when living germs corresponding to the vaccine attack the vaccinated person, the immune system is prepared. The makers of vaccines are constantly trying to find different ways to stimulate the immune system, without causing disease.
CREATING A VACCINE
Because vaccines are such a huge part of the biotechnology industry, and such an important part of our health care system, much research and money are invested in finding new and improved vaccines. Many vaccines are administered to young babies; thus, ensuring the safety and effectiveness of vaccines is critical. Many different methods of developing a vaccine exist.
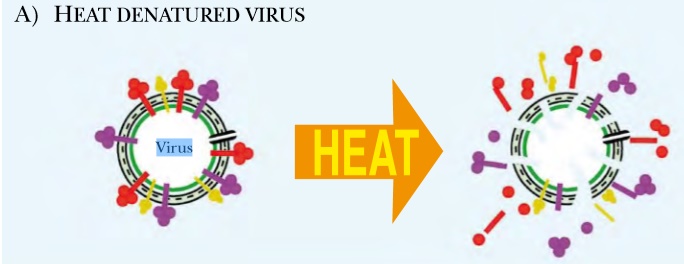
Fig 1: Whole Vaccines Include Killed
High heat or chemical treatment kills pathogens, but leaves enough antigens intact to elicit an immune response. Once exposed to a dead virus or bacterium, memory B cells are established and prevent the live pathogen from making the person sick
Heat or chemical treatment inactivates the virus or bacterium
Most vaccines are simply the disease agent, killed with high heat or denatured chemically. Heat or chemical treatment inactivates the virus or bacterium so it cannot cause disease. Yet enough of the original structure exists to stimulate immunity. When the live agent infects the vaccinated person, memory B cells are activated and the disease is suppressed. Such whole vaccines elicit the best immune response, but many diseases cannot be isolated or cultured to make whole vaccines. Other times, the cost of culturing the pathogen is prohibitive. Moreover, growing live viruses is a dangerous job, with potential exposure of lab workers. With these limitations in mind, many different strategies have been developed to make improved vaccines.
Attenuated vaccines
Attenuated vaccines are still-living pathogens that no longer express the toxin or proteins that cause the disease symptoms. Sometimes, viruses or bacteria are genetically engineered to remove the genes that cause disease. Other attenuated vaccines are related but nonpathogenic strains of the infectious agent. Making attenuated virus does not pose the same risks as for live virus. However, much research is needed to identify those genes that cause disease. Another disadvantage is that an attenuated virus might revert to the pathogenic version, especially if the attenuated virus was mutated in only one disease-causing gene.
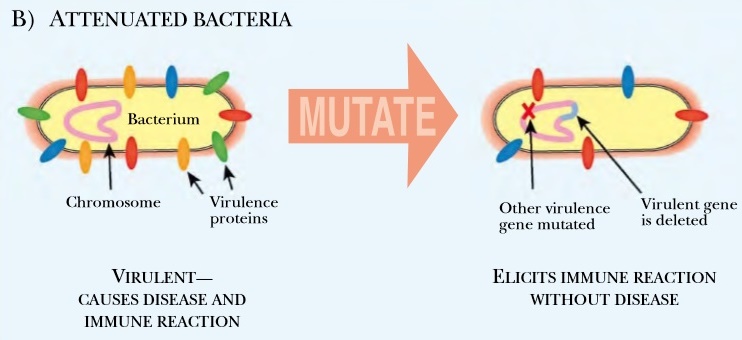
Fig:2 Attenuated Pathogens
Attenuated viruses or bacteria have been mutated or genetically engineered to remove the genes that cause illness. The immune system generates antibodies to kill the attenuated pathogen and establishes memory B cells that prevent future attack.
Subunit vaccines
Subunit vaccines are vaccines against one component or protein of the disease agent, rather than the whole disease. Subunit vaccines are available only because of recombinant DNA technology. The first step in creating a subunit vaccine is identifying a potential protein or part of a protein that elicits a good immune response.
Interior proteins from the pathogen would not trigger the immune system when the real virus challenged it. Because of this, most subunit vaccines are made from proteins found on the outer surface of the virus or bacterium.
Experiments must be done to evaluate the protein chosen for the subunit vaccine. Once a suitable protein is identified, it is expressed in cultured mammalian cells, eggs, or some other easily maintained system. The target protein is isolated from other proteins and used to immunize mice to test its effectiveness. After extensive testing in animals, the purified protein is used as a vaccine.
Sometime subunit vaccines fail, perhaps because the protein does not form the correct structure when expressed in mammalian cells or eggs. In these cases, peptide vaccines are created. These vaccines just use a small region of the protein. Since such peptides are small, they are conjugated to a carrier or adjuvant. These range from live nonpathogenic viruses or bacteria, to other proteins that stimulate a better immune response than the vaccine protein itself.